












Dental on Demand centrally provides and maintains each group’s information and customized plan configuration, which can be updated as needed. Benefits are defined by the group’s selected products and calculated with a “Benefit Period”, while the group’s determined procedure rules inform how the adjudication system processes claims. Dental on Demand also seamlessly integrates between your preferred CRM (such as Salesforce), your contacts, brokers, groups, plans, and other information.

Using group-provided member data, Dental on Demand maintains member information—especially the benefits they’re eligible for based on their group—and supports electronic eligibility processing for large national employers, as well as small businesses. Claims submitted by providers are reviewed based on the treatment services they provided to members, and the group’s rules and benefit plans. Provider payments are processed based on the member’s eligibility and services provided within a group’s plan.

Dental on Demand generates invoices using billing information from rates, miscellaneous transactions, rolling balances, and calendars. Along with processing invoices during non-production hours to ensure uninterrupted data access and updates, the system also generates extract files for printed invoices, updates your online Invoice Reprint facility for easy access by Group Administration, and seamlessly integrates with your financial system.

To support both clear results and workflows, Dental on Demand organizes reporting by each functional business area – such as Operations and Providers – and other key performance indicators, including Utilization, Lag & Incurred, and 1099’s.

Dental on Demand maintains providers by businesses, locations, licenses, networks, specialties, credentials, EFT information, holds, and comments. Third-party filed fees information is displayed in various provider management screens and utilized in claims payment generation.
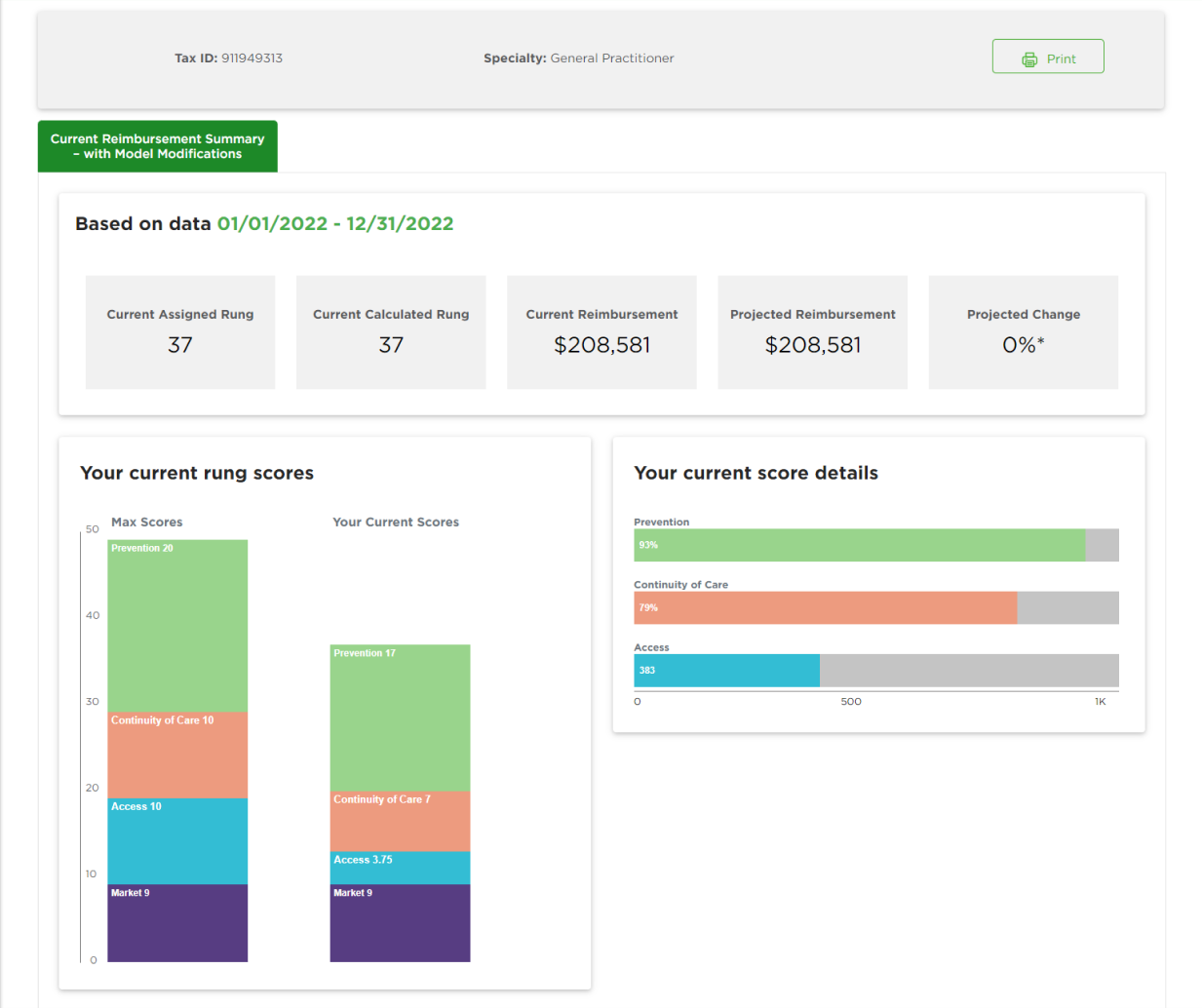
Provider’s Reimbursement Summary showcases your reimbursement success rate and gives insight into our fee-setting mechanism.
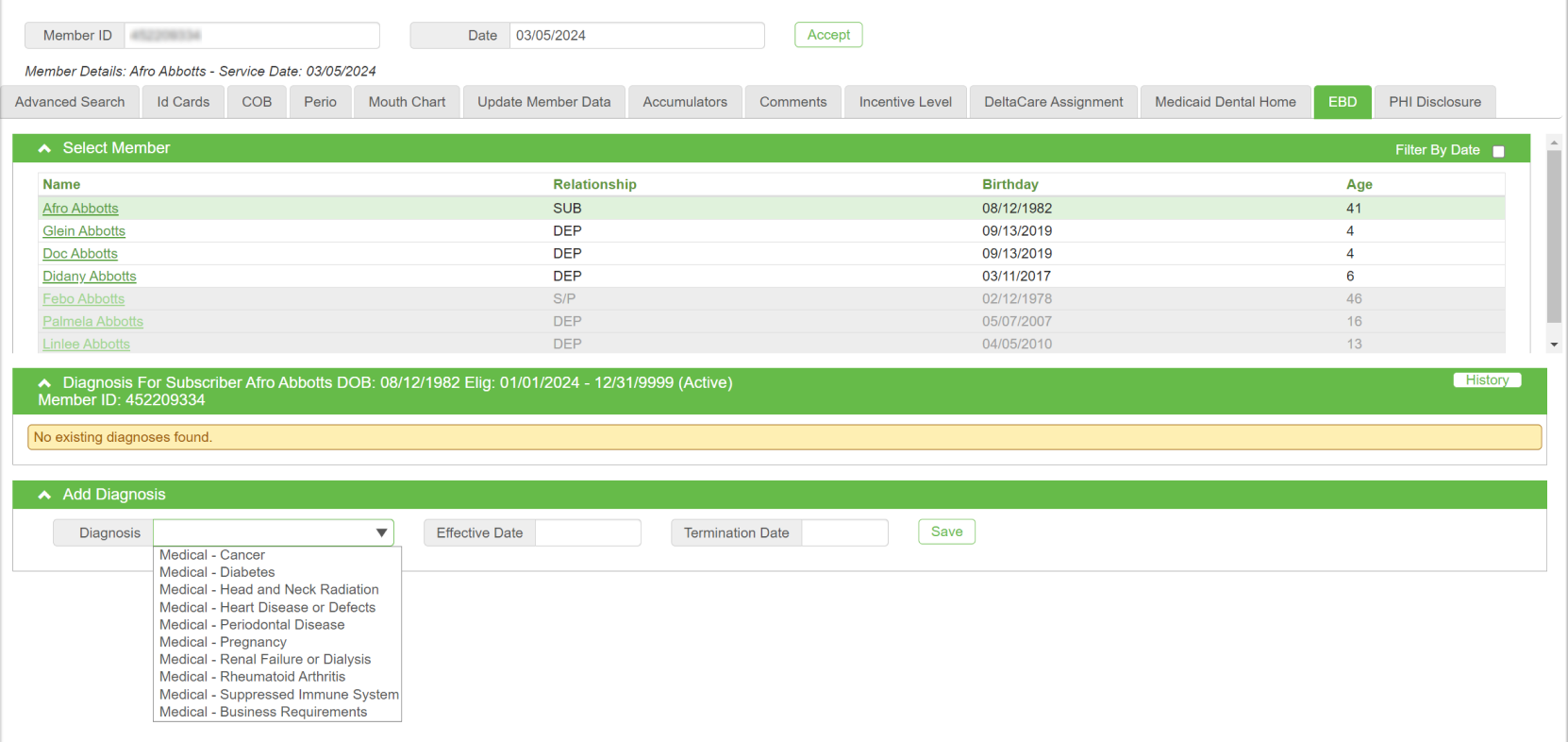
Member Diagnosis Management Screen allows the provider relations team to quickly look up a member’s diagnosis and related services. This is one example of multiple operational management screens that provide quick access to information within Dental on Demand.
Your success is our priority. To promote the highest quality experience for all stakeholders, our full-service team is here to help with training and organizational change management, tailored to integrate with your current processes, policies, and rules.
Our operational support model informs your teams with upcoming new features, supporting a culture of continual value-delivery for your stakeholders. To accelerate your learning and support your ongoing success, you're invited to join our user community and share your voice in our strategic planning and roadmap development.
“Dental on Demand (DoD) enables transparency for both Provider Relations and Operations into real-time provider data as it relates to effective dates, networks, licenses/permits and set fee schedules.”


“TriForza’s Digital Platform provides an efficient, content-managed website solution with remarkable results. Updates are completed with a few clicks, resulting in impressive speed to market and improved SEO ranking, self-service, and member/provider satisfaction.”


“Javalin’s AI reviews every radiograph from 3 clearing houses with accuracy and consistency – which was 106,000 attachments reviewed in one year.”


“Javalin’s AI-driven UM solution identified 11% more claims that did not meet clinical criteria to allow benefit payment and resulted in an increased average savings per claim reviewed by 17.4% over a 2-year period.”


“Dental on Demand is an ever-evolving application that provides visibility and manageability of Provider Data.”


“We reduced talk time minutes per subscriber by 50% using the Contact Center’s digital messaging channels along with analytics which informed automated customer experience improvements.”

