Javalin’s core modules work seamlessly together or can be purchased separately – giving you the flexibility to boost specific aspects of your utilization management and FWA operations, as well as all or a portion of your claims flow. When combined, Javalin delivers new levels of efficiencies and scale.
Claims review
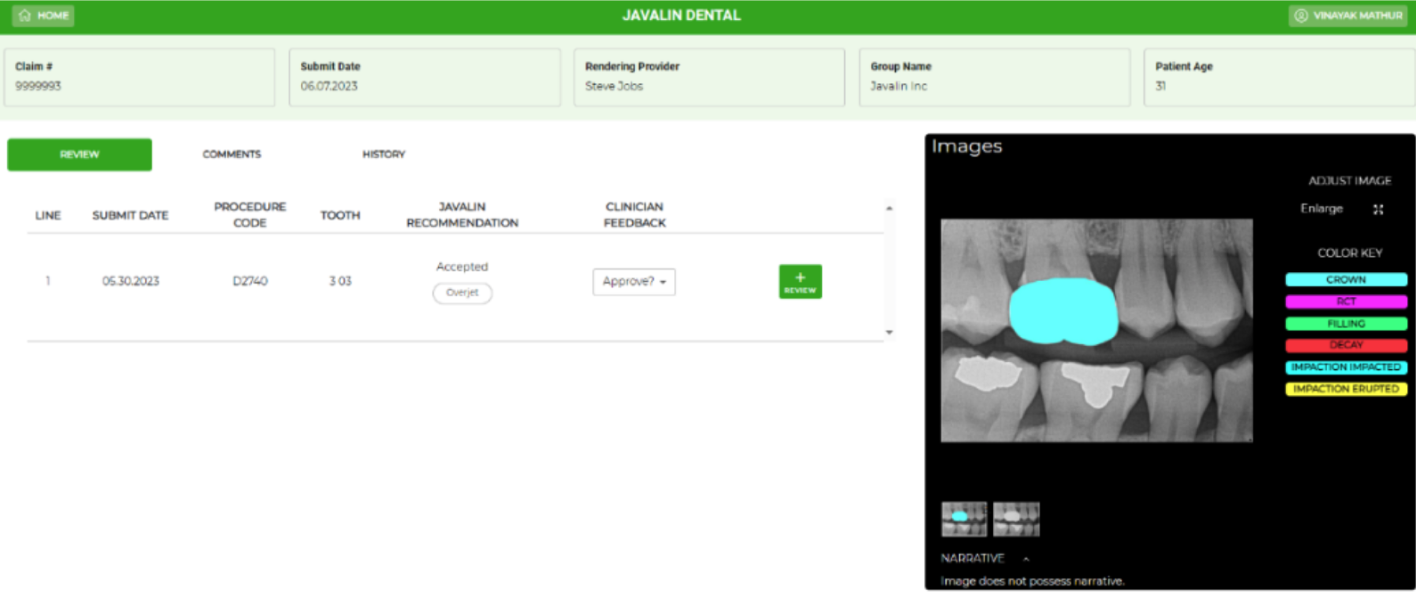
AI/ML Radiograph Review

Clinician Review
Apply heuristic analysis on claims to identify procedures for additional review
Analyze radiographs to assess compliance with payer clinical criteria
Licensed dentists review claims when necessary
Apply statistical analysis on claims to identify provider outliers for audits
Analyze AI/ML clinical criteria measurements to identify provider outliers
Licensed dentists review clinical audit results when necessary
Javalin uses a combination of heuristic rules and AI-analysis to identify claims that do not meet a payer’s clinical policies. AI-analysis eliminates guesswork and provides precise, objective measurements and reasons why a procedure does not meet clinical policy guidelines.
Combining statistical rules and AI-analysis, Javalin compares providers to their peers to identify outliers, flag concerns for further investigation or audit, and provide a depth of FWA insight not previously available to payers.
Javalin ingests all claims received and applies heuristic and statistical rules to flag which procedures require clinical review. This can be established as a pre-processing step for Javalin’s AI capabilities, or a standalone service where CRS-selected claims are reviewed by payer clinicians.
Javalin is an AI-forward product that incorporates AI when appropriate into UM and FWA. By utilizing multiple AI vendors, Javalin intelligently routes which claims are sent to which vendors, based on vendor expertise, to optimize automated review recommendations.
For payers that would like to outsource all or a portion of their state-licensed dentist clinical review, Javalin’s Clinician-as-a-Service (CaaS) provides a scalable solution that delivers consistent results.
Javalin’s Clinical Review Portal dramatically streamlines the review process by providing a single location for all claim review information - including radiographs and chart notes.
Javalin provides a comprehensive UM and FWA dashboard with customized reports that offer actionable insights into real-time savings, operational performance, provider network quality, and clinical review team performance.
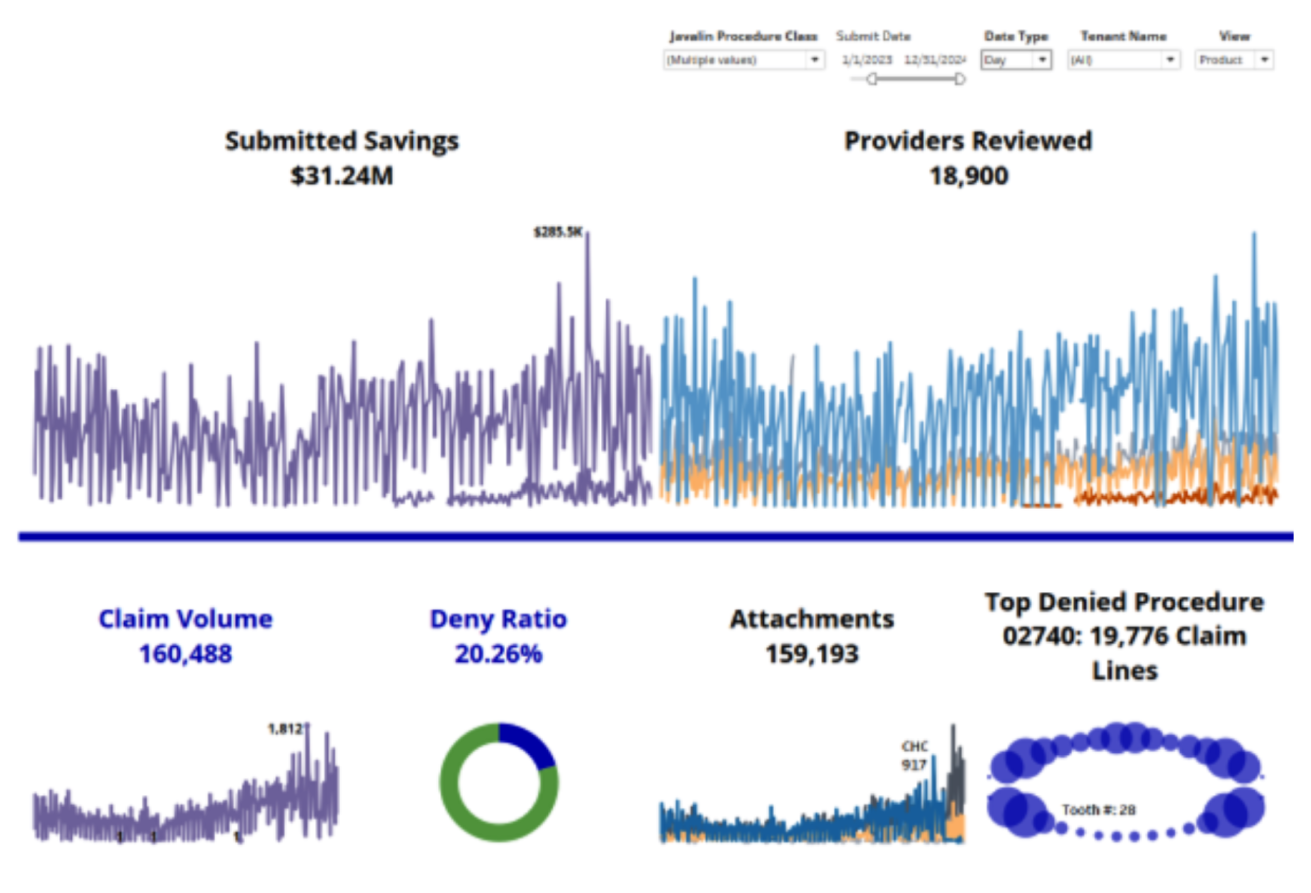
(2022 – 2023)
MILLION
Total cost savings
PERCENT
Higher savings per claim
PERCENT
Increase in clinician capacity
MINUTES
Average claim turnaround time
PERCENT
Claims identified by AI as needing clinician review
“Dental on Demand (DoD) enables transparency for both Provider Relations and Operations into real-time provider data as it relates to effective dates, networks, licenses/permits and set fee schedules.”


“TriForza’s Digital Platform provides an efficient, content-managed website solution with remarkable results. Updates are completed with a few clicks, resulting in impressive speed to market and improved SEO ranking, self-service, and member/provider satisfaction.”


“Javalin’s AI reviews every radiograph from 3 clearing houses with accuracy and consistency – which was 106,000 attachments reviewed in one year.”


“Javalin’s AI-driven UM solution identified 11% more claims that did not meet clinical criteria to allow benefit payment and resulted in an increased average savings per claim reviewed by 17.4% over a 2-year period.”


“Dental on Demand is an ever-evolving application that provides visibility and manageability of Provider Data.”


“We reduced talk time minutes per subscriber by 50% using the Contact Center’s digital messaging channels along with analytics which informed automated customer experience improvements.”

